Curriculum at a Glance
The University of Arizona Department of Pediatrics Residency Training Program provides a combination of progressive educational experiences and increasing patient care responsibilities. A wide variety of diagnoses is assured from local, regional, state-wide outreach clinic and national referrals. Extensive elective and research opportunities augment core rotations. We currently run on a 4-week block rotation schedule comprising 13 individual experiences for residents.
There are patient caps on all inpatient services ensuring maximal education and excellent patient care.
policies_and_procedures_2022-23.pdf
Post-Graduate Year 1 (PGY-1)
The first year of residency is designed to provide a comprehensive experience in inpatient and outpatient pediatrics; a basic foundation of knowledge of human growth and development and pediatric diseases; and an opportunity to develop the basic clinical and technical skills involved in the diagnosis and treatment of illnesses and diseases of infants, children, and adolescents.
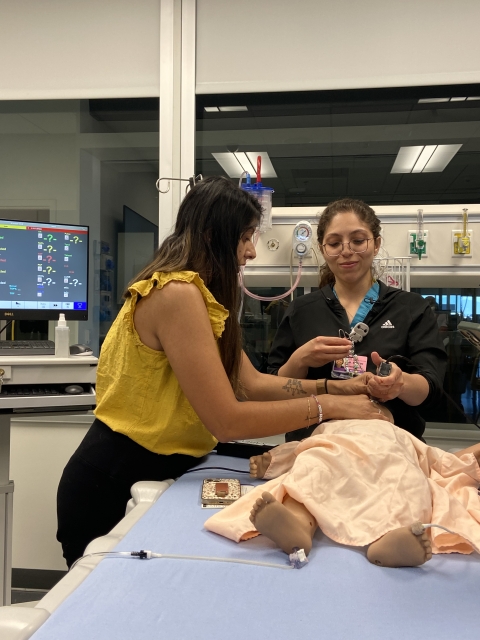
The PGY-1 year is preceded by a 2 week-long orientation to ease the transition from medical school to internship. Certification in Pediatric Advanced Life Support (PALS) and training in Neonatal Resuscitation Program (NRP) are obtained during this time.
First-year residents rotate through the inpatient pediatric wards, the neonatal intensive care unit, the normal newborn nursery, and the hematology/oncology service at Banner-University Medical Center-Tucson (BUMCT). Rotations in the ambulatory clinics take place at BUMC-Children's Multispecialty Center. All PGY-1s have rotations in adolescent medicine and one core elective of their choice. Each resident establishes their own weekly continuity clinic, which extends throughout the training program.
The PGY-1 is the primary physician for pediatric patients. The PGY-1 also has the responsibility for teaching medical students. The resident completes the initial patient history, performs the physical examination and, after consulting with the senior resident and attending faculty, writes the appropriate orders.
There is no rotating q3 or q4 call on any rotation, and no 24 hours call for PGY-1s. PGY-1s will be assigned to provide back up for their colleagues on the wards.
- Clinic: 2 blocks
- Wards Days: 3 blocks
- Wards Nights: 1 block
- Emergency Medicine: 1 block
- Heme/Onc: 1 block
- Newborn Nursery: 1 block
- NICU: 1 block
- Adolescent Medicine: 1 block
- Elective: 1 block
- Vacation 1 block
Post-Graduate Year 2 (PGY-2)
This year provides an opportunity for resident physicians to improve their clinical skills and to assume increasing levels of responsibility for patient care, as well as the supervision and teaching of first-year residents and students. PGY-2s also expand their knowledge and skills in emergency medicine and subspecialty areas.
Inpatient rotations include inpatient wards, and pediatric and neonatal intensive care units. Ambulatory medicine experience is obtained at BUMC-Children's Multispecialty Center. For those pursuing the ambulatory pathway a community site may also be available. The Behavior/Development rotation provides experience with a wide variety of children who are at risk for, or diagnosed with a genetic, neurodevelopmental or behavioral condition. Please see Pathway Description for more information on pathways.
Night call during the PGY-2 year is 1-2 times per month. There is no rotating q3 or q4 call on any rotation. There is one call free block during which residents can pursue away, rural, or international rotations.
- Clinic: 1 block
- Wards Days: 1 block
- Wards Nights: 1 block
- Emergency Medicine: 1 block
- Heme/Onc: 1 block
- NICU: 1 block
- PICU: 1 block
- Developmental And Behavioral Pediatrics: 1 block
- Elective: 3 blocks (1 block Call Free)
- Research/QI: 1 block
- Vacation: 1 block
Post-Graduate Year 3 (PGY-3)
Physicians in their third year assume maximum responsibility for patient care as well as the supervision and teaching of junior house officers and medical students. In addition to inpatient and outpatient rotations, PGY-3s are provided with extensive elective time and experience. Night call during the PGY-3 year is 1-2 times per month. There is no rotating q3 or q4 call on any rotation. There is one block during which residents can pursue away, rural, or international rotations.
- Clinic: 2 blocks
- Wards Days: 1 block
- Nights: 0.5 blocks
- Newborn Nursery: 0.5 blocks
- NICU: 1 block
- PICU: 1 block
- Emergency Medicine: 1 block
- Elective: 4 blocks (1 Call Free block)
- Career Confirmation Elective (CCE): 1 block (leadership experience)
- Vacation 1 block
Continuity Clinic:
Each resident is assigned one half-day of continuity clinic each week. Prior to beginning their first year, interns are able to rank their continuity clinic preferences. There are multiple different site options: Banner University North Hills Academic General Pediatrics Clinic, El Rio Community Health Center General Pediatric Clinic, or one of several private general pediatric practices in the Tucson area. While all clinics provide continuity experience in ambulatory pediatrics, each clinic has unique patient populations.

